DIAGNOSIS
Knowing if a person is having a seizure and diagnosing the type of seizure or epilepsy syndrome can be difficult. There are many other disorders that can cause changes in behaviour and can be confused with epilepsy. Since the treatment of seizures depends on an accurate diagnosis, making sure that a person has epilepsy and knowing what kind is a critical first step.
Neurological examination is a key step in the diagnosis.
Clinical history and neurological examination are the basis for the diagnosis of seizures and, consequently of epilepsy. Often the doctor asks for a laboratory evaluation (tests), but they are considered as additional diagnosis tests. Blood tests are used to check your global Health status and to screen for any other medical condition that may be the cause of epilepsy.
The history of the characteristics of the disease is the first important step in diagnosis.
The history of the characteristics of the disease is the first important step in the diagnosis. The doctor needs all the information about what happened before, during, and after your seizures, so he will probably ask about the premonitory signs and the details of the seizure (how it happened, duration, feelings and sensations before, during and after the epileptic seizure). If you cannot give enough information, then others who have seen the seizures happen should contribute what they know.
EEG | ELECTROENCEPHALOGRAM
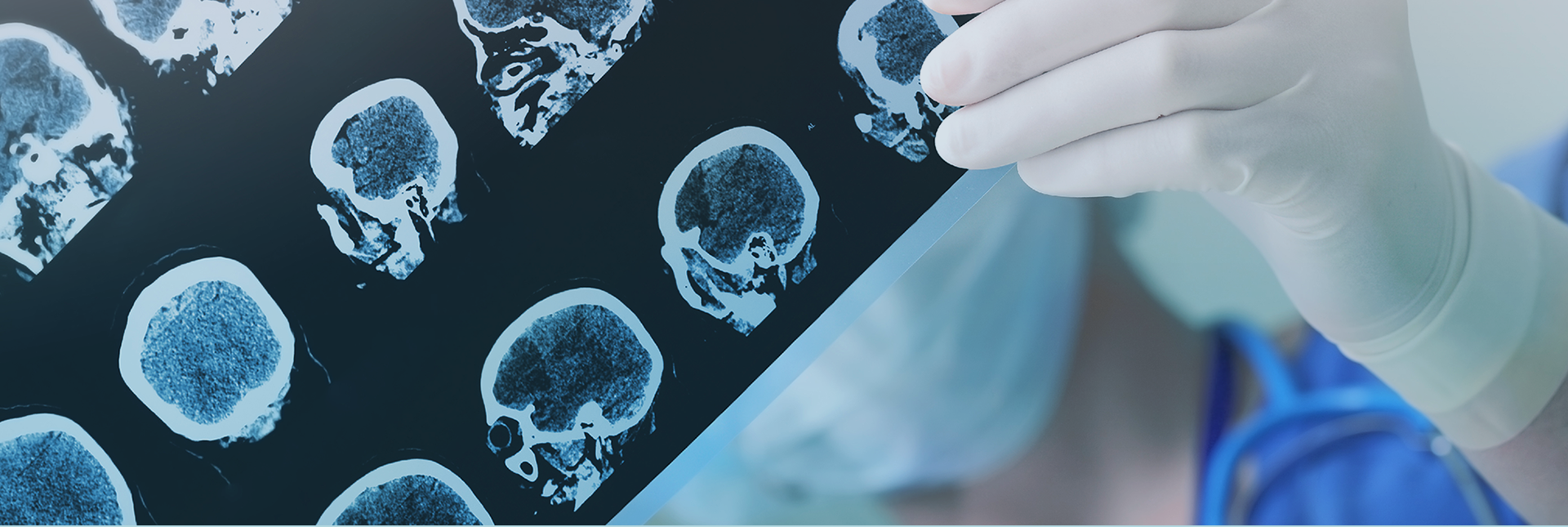
CT SCAN | COMPUTED TOMOGRAPHY SCAN
MRI | MAGNETIC RESONANCE IMAGING